With the enhanced Affordable Care Act (ACA) premium tax credits set to expire soon, many people could see their marketplace plan premiums rise in 2026. As a result, some may consider switching to a high-deductible health plan (HDHP) to keep monthly costs manageable.
An HDHP keeps your monthly premiums low while typically providing 100% coverage for in-network preventive services before you meet your deductible. Sounds good, right? But it’s not quite that simple.
An HDHP can save you money up front, but it also comes with higher out-of-pocket costs if you need medical care beyond routine checkups. In this guide, GoodRx explains how this type of plan works to help you decide whether an HDHP is the right fit for your budget and healthcare needs.
Key takeaways:
An HDHP is a health insurance plan with a high deductible and, typically, lower monthly premiums compared to a traditional health insurance plan. A health plan deductible is the amount you pay out of pocket for medical care before your insurance covers any costs. A premium is what you pay every month for your plan.
More specifically, an HDHP is a plan with a deductible that meets or exceeds the minimum annual amount set by the federal government.
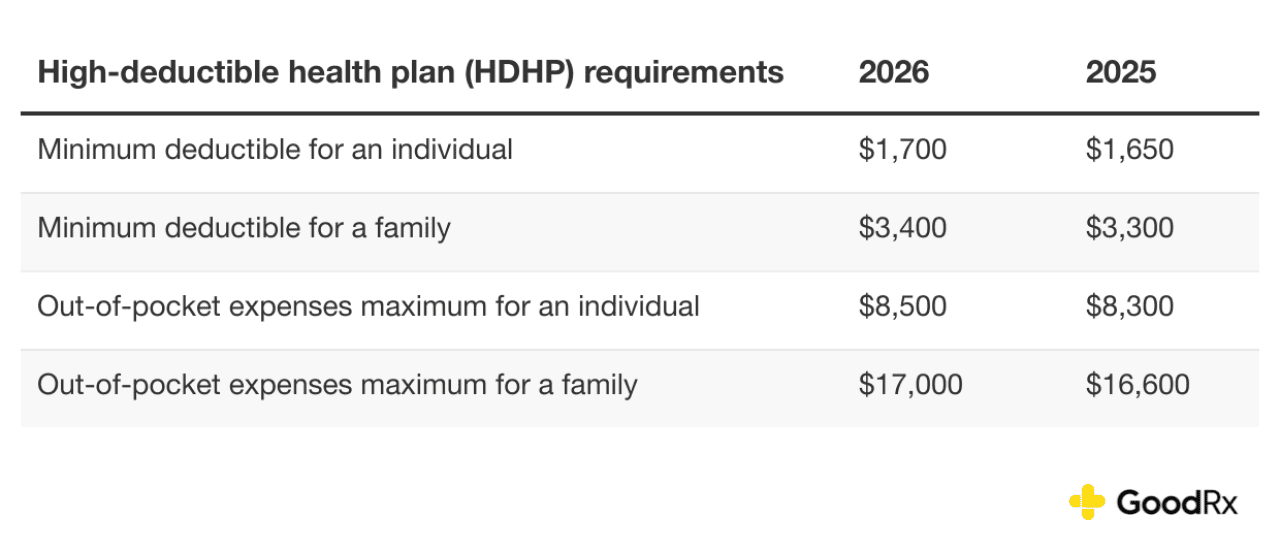
To qualify as an HDHP in 2026, a plan must have a deductible of at least $1,700 for individual coverage or $3,400 for family coverage. These plans also have out-of-pocket spending maximums, which include coinsurance, copays, and deductibles, but not premiums. In 2026, spending is capped at $8,500 for an individual and $17,000 for a family.
If you reach your out-of-pocket maximum, your plan will pick up 100% of your costs for the rest of the calendar year. But keep in mind that the limit does not apply to services outside your network.
The table below shows HDHP minimum deductibles and maximum out-of-pocket expenses for 2025 and 2026.
If you’re enrolled in an HDHP, your in-network preventive care is covered without you having to pay the deductible first. Because of this, a high-deductible plan can be a smart financial decision.
An HDHP may also cover some telehealth or virtual care visits before you meet your deductible. Under the One Big Beautiful Bill Act (OBBBA), a permanent safe harbor lets plans do this without affecting enrollees’ health savings account (HSA) eligibility. This rule applies to plan years beginning after Dec. 31, 2024.
A list of preventive services and screenings covered by HDHPs is available at Healthcare.gov. Here are some examples of medical care that may be covered in full before you meet your deductible.
All marketplace plans and many other plans must cover the following preventive services for adults:
Here are some preventive services that must be covered for women with marketplace plans and many other types of insurance:
These preventive services must be covered for children under marketplace and most other health plans:
Here are some of the benefits of an HDHP.
Effective Jan. 1, 2026, the OBBBA expands HSA eligibility by reclassifying bronze and catastrophic ACA marketplace plans as qualifying HDHPs. Bronze plans are the lowest-cost metal tier plans and typically come with higher deductibles. Catastrophic plans are very high-deductible options available to people under 30 and those with a hardship exemption.
Yes, HDHPs keep monthly payments low. But there are some downsides you should consider, including the following.
You can’t tell if or when a medical disaster may strike, so picking a health plan is always a bit of a gamble. If you need emergency care, you’ll have to pay your deductible up front, and you may have costs beyond that, up to your out-of-pocket maximum. So be sure to also look at a plan’s out-of-pocket maximum — and determine if you have access to that amount of money — before enrolling.
Whether a plan with a high deductible or one with a low deductible is better for you depends on your individual needs. HDHPs typically have lower monthly premiums. These plans are ideal for people who are generally healthy and do not expect to visit a healthcare professional often. An HDHP can also be paired with an HSA. By contributing to an HSA, you can take advantage of triple tax benefits and save money on healthcare now and during retirement.
Plans with lower deductibles may have higher monthly premiums. Like HDHPs, these plans usually cover preventive services up front, but you likely won’t have to pay as much out of pocket before your coverage kicks in for additional care.
In short, if an HDHP covers your annual preventive care and you think that’s all you’ll need in a given year, it may make sense to enroll. But if you’re worried about needing other kinds of care, it may make sense to pay more in premiums each month for a plan that offers more immediate access to comprehensive coverage.
You may have the option to choose between an HDHP and a preferred provider organization (PPO) plan. These plans work differently, especially when it comes to costs. Here’s a chart comparing the features of these plans to help guide your decision.
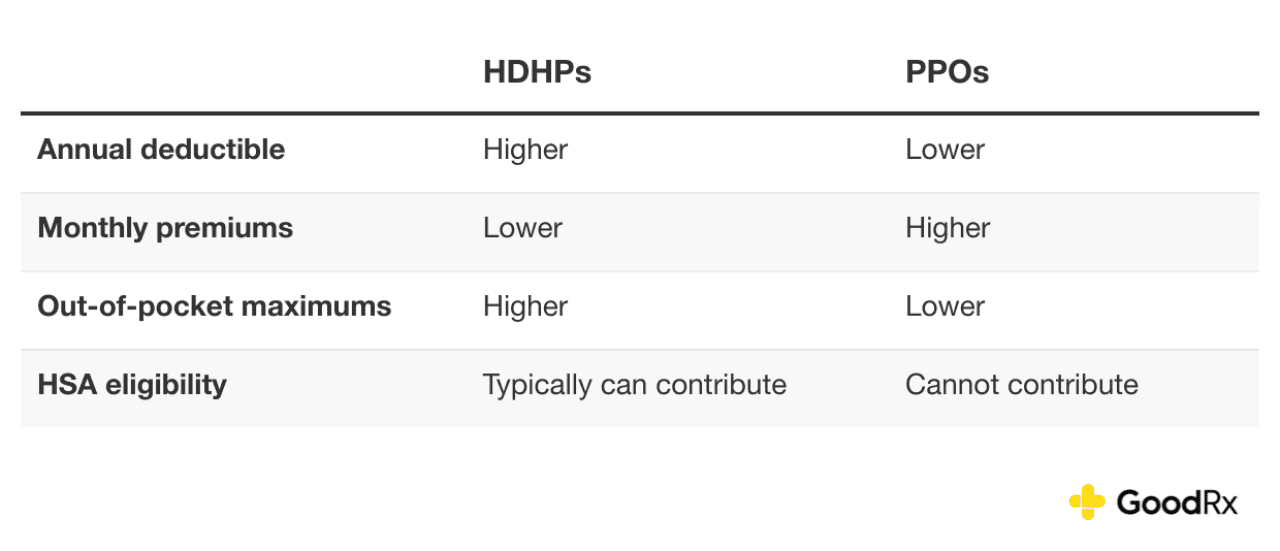
Since HDHPs have a higher deductible and lower monthly premiums, you’ll have to pay more out of pocket for certain types of medical services before your coverage kicks in. PPOs, on the other hand, have a lower deductible and higher monthly premiums, and they have lower out-of-pocket costs for medical services.
With a PPO, you may have access to a larger pool of providers and hospitals, and some out-of-network coverage. Another PPO perk is that, in most cases, you won’t need your primary care provider’s approval to see a specialist or have a test done. In general, PPOs tend to offer more flexibility, but you pay for it in premiums.
A high-deductible health plan (HDHP) may be able to help you save money by allowing you to pay lower premiums and giving you access to a health savings account (HSA). This is especially true if you are generally healthy and the plan covers all of your routine care.
But HDHPs aren’t right for everyone. If you need ongoing medical care or face unexpected health issues, you may wind up spending more out of pocket with an HDHP. And while more Affordable Care Act (ACA) marketplace plans will qualify as HDHPs starting in 2026, your best bet is to crunch the numbers based on your individual financial and health status to see which options may be best for you.
This story was produced by GoodRx and reviewed and distributed by Stacker.
Reader Comments(0)